Living with someone who has an LVAD. It’s hard adjusting to a New Way of Life. Not only for the LVAD recipient but also for the one’s around them! It’s not always easy. So many instant changes that change your everyday routine for life. And the hardest thing for us was Understanding it and then Learning it. This device is not known to the public like a heart transplant is. But it really should be.
This is my Husband’s Journey:
It all started about 8 years ago when he was having trouble walking behind the lawnmower. He was always out of breath and feeling tired all the time. It was becoming harder and harder for him to finish the yard like normal. That’s when we made an appointment with his Doctor. At that time they discovered that he had Congestive Heart Failure, and at that time his heart was working at about 30%. They recommended that he get a Pacemaker/Defibrillator. After surgery he started feeling much better. Life for him resumed as normal. Now fast forward 8 years. We were on Vacation with some of our Family and Friends.
I remember it so clearly, it was a Sunday and we were getting ready for a seafood boil down the street. It was between 85-90 degrees that day. My husband was doing ok, but just said he was feeling a little off. After we were done eating he wanted to go home and get into the air-conditioning. That made me a little suspicious, because he loves the heat more then I do. I began to wonder if he was getting dehydrated. Prior to Sunday he had been golfing with his buddies and it was a pretty hot week altogether. So I went and got him some Pedialyte to bring up his electrolytes. Shortly after drinking it he wanted to go to bed for the night. I found it strange because it was 6:30 PM, the man has never even napped in all the time I’ve known him.
The call no one wants to get!
The next morning we received a call from the Pacemaker monitoring office. My husband had a Cardiac Arrest at 2 AM and they wanted to know how he was feeling. (Basically, he died in his sleep and his pacemaker did its job and revived his heart). To their surprise, he never felt a thing. Thank God, for that Pacemaker.
They asked him to do a self test with the machine so they could take another reading. Within minutes they called us back and told us to go right to Emergency at the nearest hospital. After many tests, they decided to keep him in the hospital. After 5 days they told us there was nothing more they could do for him and that he should go see his primary Cardiologist because they were having trouble keeping his heart in rhythm. With new medications they sent us on our way. Let me tell you, this is the worst kind of stress either one of us have ever had. Knowing that we had to drive 1400 miles to get home.
Once we got home we had an appointment to see his cardiologist the next day. They ran more tests and discovered that he had a blockage of 100% in the left Ventricle of his heart and that he would need a stent put in and then he should be able to go home the next day. Once the surgery was over they told us that they found 2 other arteries that they fixed instead. We were a little shocked at hearing this, we were also wondering why the doctors in Texas couldn’t have found this. This one we will never know.
Life as we know it is about to change
When I returned the next day to pick him up they informed us that they were still having trouble getting his heart to stay in rhythm and that this was a concern. They wanted to converse with other doctors about his situation. Again, to our surprise they transferred him to a Heart Hospital in Minneapolis (Abbott Northwestern) where he would spend the next 3 1/2 months. This is where we learned he would need to have an LVAD installed. The surgery for this procedure is Open Heart, just like having any kind of bypass. Let me tell you, he struggled with this for about two weeks before he gave them the ok for the surgery. He only had two options, #1, to have the surgery or #2, go home and die. I’m thankful everyday that he had the surgery.
The next 4 months were a challenge for him and for me. This process wasn’t new to us because his younger brother had an LVAD for 11 years before he was given a heart transplant. The only difference is that we didn’t live with it.
What is an LVAD?
My husband’s is a “HeartMate 3” Left Ventricular Assist Device (LVAD). This is something we both needed to get familiar with before he could be discharged from the hospital. Most of the procedures he can do himself, but sometimes he needs my assistance.
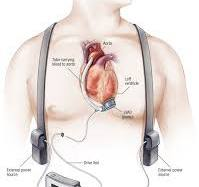
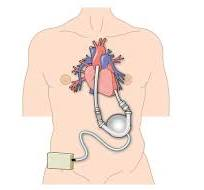
Below is what makes up the HeartMate 3 LVAD System.
- Heart Pump – Through surgery this is connected to the left side of your heart and moves blood from your heart to the rest of your body. There is a wire (driveline) that is connected to the pump and runs underneath the skin and comes out of your skin next to your belly button. This is connected to the System Controller. This can never be removed.
- Driveline – Which transfers power and information between the controller and the heart pump.
- System Controller – The System Controller is a small computer that controls and checks system information. It is connected to the pump via the driveline. It is used to control and respond to system operation. It identifies and warns him of any problems in the system operation. The System Controller consists of control buttons, lighted symbols and a user interface screen. The controller includes 15 minutes of emergency backup power.
This is how he is powered at all times day or night
- Mobile Power Unit (MPU) – The MPU plugs into an AC outlet to provide power to the HeartMate 3 LVAD System and is used when he is indoors, stationary or sleeping. The MPU transfers power to the System Controller through the units cable.
- Batteries and Battery Clips – These power the system when you are active or outdoors. You always need to use two batteries at a time.
- Battery Charger – This unit charges up to four 14 V lithium-ion batteries at a time and measures battery charge status. Each battery requires 4 hours to charge. Five lights on each battery indicate the amount of power remaining in the battery. Five being the strongest.
Most Heart Transplant Centers have these devices available.
This is the reason for the device:
This “Bridge to Transplant” device (as it is sometimes called), is used for long term therapy. Because of the circumstance’s people are having to wait for a suitable heart to become available for transplant. In my husband’s case his heart is so weak and deteriorating that it’s become unable to pump enough blood for him to sustain life. The LVAD can help the person while waiting for a heart transplant. In some cases it can also eliminate the need for a transplant. With my husband’s situation labeled “destination therapy” his will be used long-term, because he is at the end-stage of heart failure. For him it means that a heart transplant is not an option.
This is what the device does:
The LVAD has a tube that pulls blood from the left ventricle into a pump. The pump then sends blood into the aorta (the large blood vessel leaving the left ventricle). The pump is placed at the bottom of the heart inside the chest. Another tube attached to the pump is brought out of the abdominal wall to the outside of the body and attached to the pump’s battery and control system. LVADs are portable and are often used for weeks, months and even years.
Living with a Left Ventricular Assist Device – (LVAD)
This is a life altering experience. It is truly amazing what the medical industry can do and has done. This device offers hope and has extended my husband’s life expectancy because he suffers from heart failure. Living with an LVAD requires some hard to face adjustments, preparation, and a strong commitment to self care and adapting to a healthy lifestyle. However, his adjustment to the LVAD was not easy at first and he struggled sometimes with whether or not he made the right choice. But after a few months he got into a routine and a new commitment of adjusting to a new way of life.
Daily Routine with the LVAD
His morning begins with following this HeartMate log sheet daily routine. First thing he does is Performs a System Controller self test to check the audible and visual alarm indicators on the user interface. The System Controller self test is a loud, bright function. This also shows him things like the speed, flow, PI, and Power of the pump. If he can, he will take his blood pressure. (It’s not unusual to find a pulse with an LVAD patient. This is sometimes done with a Doppler in clinic). Next he will weigh himself and take his temp. Once he fills in all the boxes for the day he will begin to transfer himself over to batteries for the day. Each battery should hold a charge of up to 17 hours.
Adjusting to the Physical Changes
One of the hardest physical changes was showering. How does one take a shower with all this equipment on them? How do you protect the open wound next to your belly button? With a shower bag of course and an adhesive wound sheet protector. The shower bag keeps the controller and the batteries dry when he showers and the sheet protector helps to keep the area where the cord comes out by the belly button.
The other hardest thing for him to adjust to was not being able to swim or go into a pool ever again. This one is especially hard for him because we are pool people. Lastly, he has to bring an emergency back up bag with him where ever he goes. It’s for just in case his controller goes bad, or he may need to change the batteries.
Navigating Through Daily Life
For him, adjusting to a new routine was a little overwhelming. So many things to remember. But, as time goes on he has a pretty good routine process now. He also has more confidence in himself. Everyday I find him outside doing the things he loves that he thought he wouldn’t be able to do anymore. He’s figuring it out. Some days feel like the old days.
Rebuilding a Healthy LVAD Way of Life
We’ve been focusing on healthier habits by changing more Balanced nutritional needs, also incorporating regular exercise such as walking or riding our bikes. By focusing on his well-being helps our whole family. It’s also nice that we have support from all our family and friends. Additionally, by practicing self care, mindfulness, and positive thinking helps us contribute to his overall well-being. Progress takes time and effort. So be patient and kind to yourself throughout this journey!
Living with an LVAD is not the end of the world. It may seem like it at first, but with time it all gets easier. It’s a serious life change and you have to make the best of it. We are and everyday we are Blessed that he is still with us.
Simply Go Here and Contact Us for Additional Information. Once we add you officially into our Online Community we get to “GIFT YOU” with more and more and more! See How to Contact Us Here: